This post was submitted to us by writer Aprille Donaldson. The original post can be found on her website www.beautifulinhistime.com.
Dear CBAC Mom:
I just want you to know that I get you.
For nine months you carried your baby within you. And for nine months – maybe even longer – you dreamed about pushing that baby out of your body with your own strength.
You planned. You prepared. You hired a doula. You probably spent hours reading books and websites, making sure you were making the right choice for you and your baby.
You exercised. Maybe you changed your diet.
Maybe you had to fight. Maybe you had to drive a long way for your appointments and birth. Maybe you had to explain your choices to the naysayers.
You prayed.
At one point or another, you were probably afraid.
You wondered if you could do it. You wanted to believe you could.
You wanted to believe that this birth would be different.
But for some reason, it didn’t happen.
Your breech or transverse baby didn’t turn. The cord prolapsed. You got chorioamnionitis. Your baby went into distress. Your placenta didn’t move. Your body didn’t dilate – again. Your baby was too big, or maybe stopped growing. Your blood pressure went up. Your uterus ruptured. You pushed and pushed and that baby still. just. wouldn’t. come. out.
A call was made. and you said, “Yes…cut me open.”
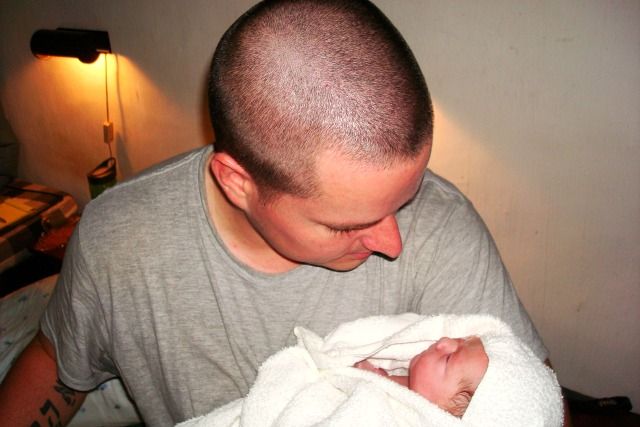
I hope that your beautiful baby is safe in your arms.
I hope that you realize how brave you are. You made a choice to try something that very few will try to do.
But when it came to the safety of your baby, you made the best choice:
You said, “I choose you!”
And that makes you a success.
I hope you know by now – I hope all of your children have taught you this:
Moms have to make hard calls. Sometimes, you have to make choices that others will judge and scorn as less than best because they are the best choices for you and your baby. Making those choices is just part of being a parent.
It’s okay to be disappointed. It’s okay to say, “This is not what I wanted.” It’s okay to grieve and cry.
But there’s no such thing as a “failed VBAC.” Because you cannot fail at birth. You cannot fail at bringing a child into the world.
Look into that baby’s beautiful face. You made that! You did that!
You are brave. Strong. Competent.
You are scarred, but you are not broken.
 This post was submitted to us by writer Aprille Donaldson. The original post can be found on her website www.beautifulinhistime.com.
This post was submitted to us by writer Aprille Donaldson. The original post can be found on her website www.beautifulinhistime.com.